Shingles on the Body
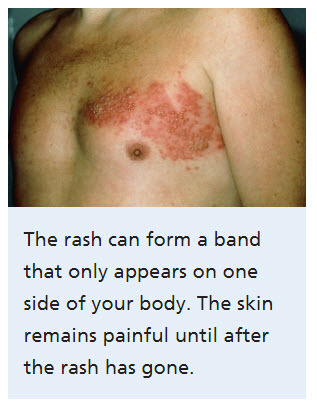
The rash and/or blisters associated with shingles most commonly appears in a strip or band formation on a single side of the body. 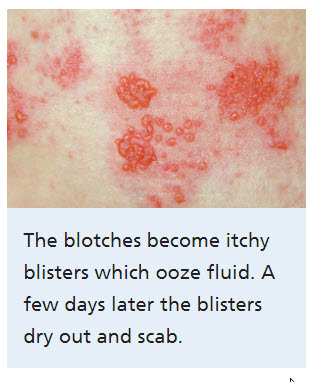
This strip or band of the shingles rash most often develops around the waist or “trunk” area.
This band follows what is called a dermatome, which is a patch of skin that is affected by one of the nerves from the spine.
Regardless, it is possible for the shingles rash to appear anywhere throughout the entire body, striking any dermatome.
The location where the rash appears is directly related to the reactivation of the virus within a particular nerve or nerves.
Postherpetic neuralgia
Postherpetic neuralgia is a complication of shingles, which is caused by the chickenpox (herpes zoster) virus.
Postherpetic neuralgia affects nerve fibers and skin, causing burning pain that lasts long after the rash and blisters of shingles disappear.
The risk of postherpetic neuralgia increases with age, primarily affecting people older than 60.
There’s no cure, but treatments can ease symptoms. For most people, postherpetic neuralgia improves over time.
Symptoms
The signs and symptoms of postherpetic neuralgia are generally limited to the area of your skin where the shingles outbreak first occurred — most commonly in a band around your trunk, usually on one side of your body.
However postherpetic neuralgia is also common in people whose shingles occurred on the face.
Signs and symptoms may include:
- Pain that lasts 3 months or longer after the shingles rash has healed. The associated pain has been described as burning, sharp and jabbing, or deep and aching.
- Sensitivity to light touch. People with the condition often can’t bear even the touch of clothing on the affected skin (allodynia).
- Itching and numbness. Less commonly, postherpetic neuralgia can produce an itchy feeling or numbness.
When to see a doctor
See a doctor at the first sign of shingles.
Often the pain starts before you notice a rash.
Your risk of developing postherpetic neuralgia is lessened if you begin taking antiviral medications within 72 hours of developing the shingles rash.
Resource
https://www.mayoclinic.org/diseases-conditions/postherpetic-neuralgia/symptoms-causes/syc-20376588
Eye
About 1 in every 7 people who develop shingles will be affected in one of their eyes.
This can look like redness and/or pain in the actual eye ball or a red rash and blisters around the eye area.
Shingles in or around the eye, called ocular shingles, can make it difficult to move the eye ball or the eyelid, as puffiness and swelling may occur.
In extreme cases, vision loss or permanent blindness can occur.
If you develop shingles in or around your eye, it is important you seek medical attention.
Face/head
A shingles outbreak may show up on your head or face.
postherpetic neuralgia
If this happens, it means the shingles virus is attacking the cranial nerves, which are the nerves that supply motor function and sensation to the head and face.
Shingles involving the cranial nerve can cause weakness of the face muscles, along with the uncomfortable rash/blisters.
Ears
Shingles near or on the ear can lead to uncomfortable complications including hearing problems, balance issues, and weakness of the facial muscles.
These symptoms may remain after the shingles rash has cleared, and can even become permanent if not treated appropriately.
Mouth
Shingles can develop in or around the mouth. Having a shingles rash in this area is especially uncomfortable, as it can be painful to eat while the rash is active.
Additionally, shingles in or around the mouth can lead to one’s sense of taste changing.
Groin
Shingles do not usually affect the groin area, but it is possible.
If you think you may have shingles in or around your groin, it is best to schedule an appointment with your doctor for purposes of accurate diagnosis and treatment.
Sometimes, other skin diseases and infections can be mistaken for shingles, including psoriasis, jock itch, pubic lice, scabies, and/or some sexually transmitted diseases.
Anus
While it is unlikely you will develop shingles in or around your anus, it is possible, as the anus contains nerve endings. 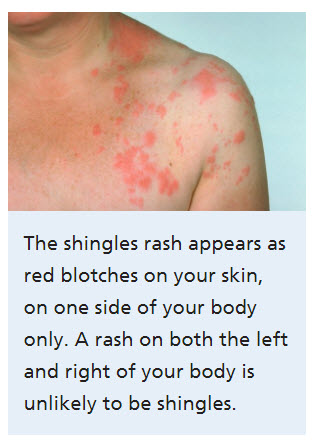
If you think you have shingles on your anus, it is important to get checked by a medical professional as soon as possible.
If not treated, this can lead to loss of sensation, incontinence, and/or retention of stool.
Nose and Scalp
The virus may also appear on the nose and scalp.
Resource
National Health Service. (2017). Shingles. Retrieved on September 11, 2017 from https://beta.nhs.uk/conditions/shingles/
Shingles without a Rash
Shingles without a rash is referred to as zoster sine herpete (ZSH).
This type of shingles is uncommon, and quite difficult to diagnose.
Causes and Risk Factors
It is unknown why the varicella zoster virus reactivates as shingles for some people and not others.
Zoster sine herpete (ZSH) or shingles without a rash is still caused by the varicella zoster virus, but like the more common shingles, only develops in some people.
Just as with herpes zoster, there are risk factors that increase ones chances of getting zoster sine herpete.
These include:
* Having HIV/AIDS
* Receiving cancer treatments (chemotherapy or radiation)
* If you are an organ transplant patient (as these individuals are usually prescribed immunosuppressant drugs)
* High levels of stress
* If you take high doses of corticoid steroids
Symptoms
Shingles without the rash is more difficult to detect, as the rash and/or blisters are not present.
Beyond the rash, ZSH does have most of the same symptoms as herpes zoster, including:
* Itchiness
* A numb feeling
* A burning sensation that is painful
* An overall achy feeling throughout the body – flu like symptoms develop in individuals with shingles (whether with a rash or not).
Muscle aches and mild fever are also common and tend to last anywhere from 7-10 days.
* Fatigue and lethargy
* Poor appetite – because of the flu-like symptoms associated with shingles, many experience a loss of appetite, which of course, can result in weight loss
* Headaches
* Pain – shingles tends to be a very painful disease.
The pain associated with shingles (with or without a rash) is usually described as a stabbing or shooting (postherpetic neuralgia pain).
Due to the impact the varicella zoster virus has on the body’s nervous system, the pain can also have an electric feel to it.
* Increased sensitivity to touch
Treatment of shingles without the rash
Once your doctor diagnoses you with ZSH, he or she will most likely prescribe antiviral medications, such as acyclovir (commonly known as Valtrex or Zovirax).
You may also be given a prescription for pain medication.
Complications of shingles without rash
Shingles with a rash (herpes zoster) typically clears up anywhere from two to six weeks after the rash develops.
Yet, in some cases, people experience pain that extends beyond the time when the rash has healed.
This is referred to as postherpetic neuralgia. And while many cases of shingles without the rash heal in a similar time frame, some studies suggest that these individuals are more likely to develop postherpetic neuralgia.
Also, those with a weakened immune system and shingles without a rash are more likely to have shingles again.
There are other complications that can result from shingles without rash, including:
* Neurological problems – the shingles virus attacks nerves, which can become permanently damaged following a shingles outbreak.
This can cause facial paralysis, hearing issues, balance problems, and/or inflammation of the brain.
* Vision loss – vision damage or permanent vision loss can occur if a shingle outbreak is in or around the eye.
These complications while rare, can be very severe, and are more likely to occur if a shingles outbreak goes untreated.
If you notice possible symptoms of shingles, but do not develop a rash or blisters, there is still a chance you have developed shingles (zoster sine herpete) and should consult with your medical professional.
Resource
Gilden, D., Cohrs, R. and Nagel, M. (2009). Neurological Disease produced by varicella zoster virus reactivation without rash. Retrieved on September 11, 2017 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3076592/
Shingles comes from the chickenpox virus that most people get as a kid.
When our immune system defeats the chickenpox virus, it traps it like a prisoner within nerve cells near the spinal cord.
Unfortunately if our immune system slips up, or gets weaker the chickenpox virus can break free.
This is why it’s more common in the elderly because they have a weaker immune system, but it can affect someone of any age.
When the virus breaks free like any prisoner it makes its way to the surface through the nervous system.
The immune system is going to do everything it can to fight this virus, and this could bring about some symptoms.
These symptoms could include a fever, a headache, diarrhea and fatigue as the body’s defense mechanism tries to stop the escaped prisoners.
Eventually the virus can make its way to the surface and will bring about a tingling sensation and the area will be sensitive to light.
Usually this tingling will take place around the stomach or chest area, but can take place anywhere.
The worst place to get Shingles is around the head area, which around 15% of people get.
The reason this is bad is because there is a lot of sensitive areas, and it could damage the eyes, causing problems and blindness.
This tingling sensation can last a few hours to weeks.
The next stage is that the tingling turns into pain.
People can experience this pain differently and it’s been described as being burning, stinging or very itchy.
It can be ongoing and could be brought on by a small breeze or light touch.
Next patches of red dots take form on the skin.
Within a day these pimples develop into tiny fluid-filled blisters.
The blisters grow and merge and become filled with this pus substance.
At this time depending on how strong the immune system is more red dots can start to appear growing the pain.
Within a week to two weeks the blisters form crusts and begin to heal.
Of course this all depends on the immune system, and it could even take months for the blisters to heal.
The good news with this health problem is that most people recover from it within a few weeks usually, but a small percentage of people get something called postherpetic neuralgia.
This is a burning sensation occurring after the rash goes away that can be so severe in gets in the way of someone’s sleeping, and there daily activity.
Right now there is no cure for this postherpetic neuralgia, but there are some treatments that help with the pain.
Shingles is usually treated with antiviral medicine and pain medicines, just like ibuprofen.
If it is treated early on it can reduce the chance of it spreading, as well as becoming postherpetic neuralgia.
The ideal way to deal with this condition is to not get it in the first place by having a strong immune system.
Strengthening your immune system not only helps a person with shingles, but with so many other problems as well.
A person can do this by eating healthy foods, getting plenty of rest and not getting stressed out a lot.
I’m not sure why stress causes the immune system to become weak, maybe it’s because the brain is so powerful that it uses a lot of energy.
There are also tons of herbal remedies and supplements that can help.
For starters green tea helps by adding interferon to someone.
Interferon interferes with a virus’s ability to replicate and that is why it has its name. Another great herb is something called olive leaf extract.
This herbal medicine is anti-viral and anti-bacterial, which can for sure help stop the growth of this ailment.
There really are just tons of others like black cumin seeds, garlic and quercetin to name a few.
To get these alternative medicines you would take a dietary supplement product.
In case you haven’t noticed supplements can be confusing because there are so many of them that all say the same things.
To make matters worse government agencies like the FDA in the U.S. don’t regulate the industry, so it’s easy for companies to make crappy products.
Why Some People Get Shingles and Others Do Not
The varicella zoster virus (VZV), which is one of eight herpes viruses known to infect humans, causes both chicken pox (varicella) and shingles (herpes zoster).
Chicken pox results from one’s initial exposure to the virus (and usually occurs in childhood).
Once a person has had chicken pox, the virus remains in his or her body’s nerves indefinitely.
When the varicella zoster virus is reactivated, shingles develop.
Thus, only people who have previously had chicken pox can develop shingles (this includes children as well).
Around 1 million people suffer from shingles each year, which is approximately 30% of people who have had chicken pox.
Unfortunately, the reason the varicella zoster virus only reactivates for some is not well understood.
Risk Factors
Nonetheless, there are some factors that will increase one’s risk of developing shingles.
Most risk factors (or factors that increase the chance of triggers a shingles outbreak) revolve around decreased function of the immune system, including:
* Age – although a person of any age can get shingles, as he or she ages, the risk of developing shingles increases.
* Cancer treatments – chemotherapy and radiation are shown to lower a person’s resistance to disease, infection, etc.
* Certain medications – immunosuppressive drugs lower the one’s immune system function, making them more susceptible to developing shingles
* Diseases – HIV/AIDS and certain cancers
* Children – children are more likely to develop shingles if their mother had chicken pox late in the pregnancy or if the child had chicken pox as an infant.
Other possible factors
There are other hypotheses about what can trigger the reactivation of the varicella zoster virus.
One of the most widely discussed is the possible connection between stress and shingles outbreaks.
The immune system and central nervous system are interconnected.
Thus, it is logical to suggest physical and/or psychological stress can affect these two systems operative interactions, resulting in a weaker immune system, and subsequent shingles.
* Physical stress – many people suffer from chronic pain (because of various medical conditions).
Because chronic pain can be a significant stressor, it is thought that this may trigger a shingles outbreak.
* Psychological stress – also known as emotional stress, can also affect the body’s ability to defend against illness and virus.
The duration and intensity of stress are likely related to the level of resulting immune dysfunction.
Of course, stress is just a factor that increases one’s risk of developing shingles.
It is not a cause of shingles (remember, for those who develop shingles the virus is already lying dormant in the body).
Although it is inconclusive as to exactly why some people develop shingles and some do not, it is clear certain factors greatly increase an individual’s risk.
While most people who do develop shingles only experience one outbreak, some do have a second or third episode at some point throughout their lifespan.
Resource
Pergam, S. & Limaye, A. (2009). Varicella zoster virus. Retrieved on September 8, 2017

